Get to know osteoporosis
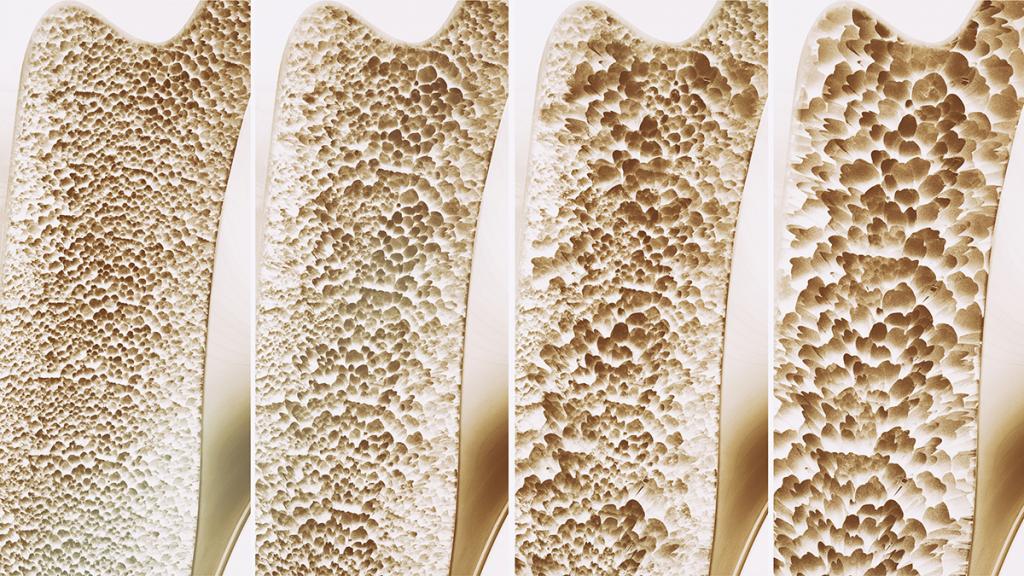
Osteoporosis is a bone disease that gradually develops when bone mineral density or bone mass decreases and the quality of bone is impaired. As a result, it can lead to a decrease in bone strength and increase the potential risk of fractures. Osteoporosis causes bones to become weak and brittle, therefore even minor trauma or mild stress can cause a fracture. Moreover, osteoporosis in the spine often leads to loss of height over time. Osteoporosis frequently refers to “the silent killer” since it usually exhibits no symptoms. The patients are unaware of their bone loss until they experience fractures.
Most commonly affected areas
Osteoporosis-related fractures most commonly occur in
- Spine
- Hip
- Wrist
Warning signs and symptoms of osteoporosis
There typically are no warning symptoms in the early stages of osteoporosis. Patients are aware that they have osteoporosis when bones are broken due to accidents or other forms of traumatic injuries.
However, once the bones have been weakened by osteoporosis, related signs and symptoms that need medical attention include:
- Back pain, caused by a collapsed spine
- A stooped posture
- Loss of height over time
Cause of osteoporosis
Bone is comprised of both osteoblasts and osteoclasts. Osteoblasts are the cells required for bone synthesis and mineralization, both during the initial formation of bone and during bone remodeling. While osteoclasts are cells that break down bone, responsible for bone resorption. Bone metabolism is a continual cycle of bone formation and bone resorption that is carefully orchestrated by the dynamic relationship between osteoblasts and osteoclasts. Osteoporosis is a metabolic bone disease that, on a cellular level, results from the imbalance of bone formation and bone resorption, causing more bone destruction. As a result, bones become weak and fragile, thus increasing the risk of fractures. The causes of imbalance of bone hemodynamics often involve the insufficient amount of calcium that is required for bone formation and abnormal bone cells.
Risk factors of osteoporosis
A number of factors increase the chance of developing osteoporosis, including:
- Increasing age. People with advancing age are at greater risk of developing osteoporosis. Since the bones become fragile and brittle, even mild stress or traumatic injury can susceptibly lead to fractures.
- Estrogen deficiency in post-menopause women or decreased level of testosterone in men. Estrogen deficiency can lead to excessive bone resorption accompanied by inadequate bone formation.
- Family history. Having a parent or sibling with osteoporosis puts increased risk of osteoporosis, especially if mother or/and father have history of a fractured hip.
- Abnormal functions of certain glands or organs e.g. thyroid gland, parathyroid gland, adrenal gland, kidney and liver.
- Certain diseases or conditions e.g. autoimmune diseases, such as systemic lupus erythematosus (SLE) and rheumatoid arthritis as well as bone cancer.
- Low calcium intake. A lifelong lack of calcium plays a significant role in the development of osteoporosis. Low calcium intake contributes to reduced bone density, early bone loss and an increased risk of fractures.
- Long-term use of some medicines that interfere with the bone-rebuilding process such as oral or injected corticosteroid medications.
Complications of osteoporosis
Potential complication caused by osteoporosis is pain which is the result of nerves being pinched as the muscles tense to protect the joints and in turn the bones. The most common cause of osteoporosis pain is a spinal compression fracture which induces sudden, severe back pain that largely restricts mobility and interferes with daily activities. Due to impaired quality of life, this can eventually lead to depression and other mental health problems. Moreover, affected bones become more susceptible to break even with mild physical stress or injury. Hip fractures from osteoporosis are usually the result of a fall. It commonly occurs in elderly people, leading to severe hip pain, restricted movement and inability to walk. If left untreated, patients with hip fractures are at greater risk of immobilization and being bed-ridden, leading to other serious complications, such as bedsores (pressure ulcers) and urinary tract infections.
Diagnosis of osteoporosis
Test to diagnose osteoporosis involves bone density test which is an imaging test using small amount of X-rays to determine the mineral density of the bones. This non-invasive test aims to measure the strength of the bones while using less time consumption. Bone density test is considered highly effective to diagnose osteoporosis before a broken bone occurs. This test also helps to estimate chance of breaking a bone in the future, allowing for appropriate and timely intervention and treatment planning at earliest stage before any symptom arises. The result of bone density test refers to the bone mineral density (BMD). BMD of healthy people is greater than -1. While people with reduced bone mass (osteopenia) have BMD between -1.0 to -2.5 and people with osteoporosis have BMD lower than -2.5.
Treatment of osteoporosis
Several factors contribute to osteoporosis. The goals for treating osteoporosis are to slow bone loss and prevent fractures. Therefore treatments aim at improving bone formation and reducing bone resorption. There are several medications used to prevent or treat osteoporosis. The specialist selects the most appropriate option, taking into consideration patient’s conditions and general health as well as the amount of bone loss and an estimated risk of breaking a bone. Regardless of medication type, it remains important to regularly consume recommended amounts of calcium and vitamin D in combination with exercise. Treatments practically involve oral medications, injections and hormonal drugs.
- Medications: Several medications are available in oral dosage form and injections. These medication are, for example:
- Alendronate: Alendronate inhibits osteoclast activity, thus slowing down bone resortion. In addition, it increases the amount of calcium in the bones (bone mineral density), making stronger bones and less likely to break.
- Risedronate: Risedronate is also powerful bone resorption inhibitor. By slowing down the rate at which bone is dissolved, risedronate increases the amount of bone, leading strengthened bone and reduced risk of fractures.
- Ibandronate: Similar to alendronate and risedronate, ibandronate inhibits osteoclast function, leading to reduced bone loss. Both oral tablet and intravenous injection forms are available.
- Zoledronic acid: Via intravenous injection, zoledronic acid helps slowing down bone resorption process and inhibiting the release of calcium into blood circulation, thus preventing high blood calcium level (known as hyperkalemia).
- Hormonal therapy: Hormonal therapy such as estrogen is approved to prevent osteoporosis and fractures in postmenopausal women or women who cannot produce sufficient level of estrogen such as women who have had uterine and ovary removed.
Prevention of osteoporosis
Good nutrition and regular exercise are essential for keeping bone healthy and preventing osteoporosis. Maintaining a healthy lifestyle includes:
- Consume diets with high calcium and vitamin D
- Stop or reduce smoking, if smoke
- Avoid drinking alcohol, soft drinks, tea, coffee or caffeine-containing beverages or acidic drinks
- Exercise regularly
- Maintain healthy weight
- Avoid taking certain medications, especially long-term use of corticosteroid drugs
In addition, studies have shown that soy isoflavones combined with calcium intake may prevent osteoporosis and improve bone strength, thereby decreasing the bone resorption and decreasing risk of fracture, especially in menopausal women.