Hip pain is a common issue that affects people of all ages and activity levels. Misconceptions about its causes and treatments often lead to confusion and ineffective management. This article aims to provide accurate information to help you better understand your hip health. Let’s explore some prevalent myths about hip pain and uncover the facts.
Myth 1: If You Experience Hip Pain During Movement or Exercise, There Must Be Something Wrong with the Joint Itself
Fact: Hip pain is a complex issue with a wide range of potential causes. The location of the pain plays a crucial role in determining its origin. Pain in areas such as the groin, side of the hip, buttocks, or even near the perineum can indicate different underlying problems. The discomfort may originate from muscles, tendons, bursae (fluid-filled sacs that cushion joints), or issues within the joint itself. Sometimes, minor joint problems can cause compensatory stress on surrounding structures, leading to pain. A precise physical examination and accurate diagnosis are essential to identify the true cause and provide effective treatment.
Myth 2: Hearing Sounds from Your Hip Indicates Cartilage or Bone Damage
Fact: Hearing a clicking or snapping sound in your hip doesn’t necessarily mean there’s damage to the cartilage or bones. Often, these sounds are associated with a condition known as snapping hip syndrome, which can be classified as internal or external. This syndrome is usually caused by muscles or tendons moving over bony structures and can often be managed with targeted physical therapy to address muscle imbalances and reduce inflammation. However, it’s important to note that while snapping hip syndrome is a common cause of hip sounds, it doesn’t entirely rule out joint pathology. A thorough evaluation is necessary to exclude other potential issues.
Myth 3: If You’re Young and Active with Hip Pain, You Should Train More to Improve Hip Stability and Function
Fact: While maintaining an active lifestyle is generally beneficial, increasing training intensity without understanding the cause of your hip pain can be counterproductive. It’s crucial first to determine whether the pain is due to bone pathology, cartilage involvement, a labral tear, or soft tissue inflammation. Continuing high-intensity activities may exacerbate inflammation and lead to a cycle of worsening pain. Reducing the intensity of your workouts can help decrease inflammation. Light-intensity exercises can maintain mobility, muscle mass, and function without overloading the joint. Specific treatments should be tailored to the underlying pathology. A proper diagnosis, which may require medical imaging or other interventions, is key to successful management.

Myth 4: Osteoarthritis or Degenerative Changes in the Hip Joint Only Occur in Older Adults
Fact: Contrary to popular belief, osteoarthritis and cartilage damage in the hip can occur in younger patients, often due to secondary causes. Unlike knee osteoarthritis, which is typically age-related, hip osteoarthritis in young individuals is often linked to:
- Hip Dysplasia: This condition involves a shallow hip socket and can be present from childhood. Symptoms may not appear until adulthood, leading to early degeneration.
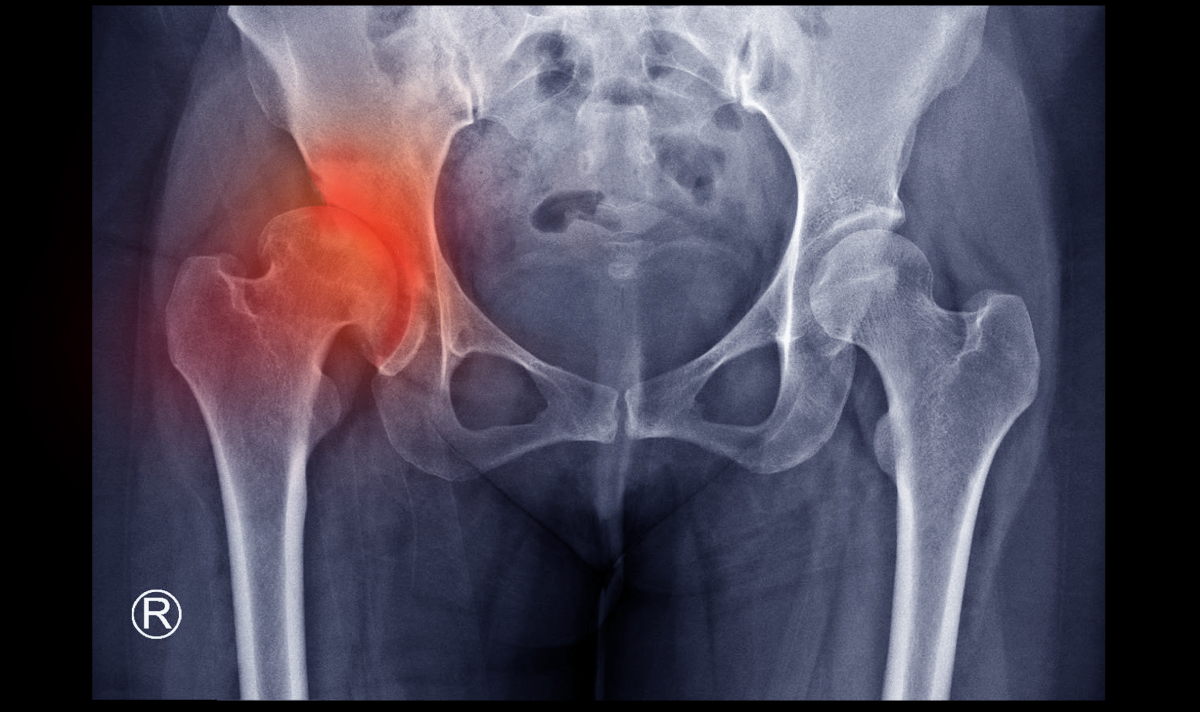
- Osteonecrosis of the Hip: Poor blood supply to the femoral head can cause bone tissue death. Causes include long-term steroid use, excessive alcohol consumption, systemic lupus erythematosus (SLE), certain infectious diseases, blood clotting disorders, sickle cell anemia, or prior injury. The femoral head may lose its spherical shape, resulting in improper joint movement and osteoarthritis.
- Femoroacetabular Impingement (FAI): Abnormal bone shapes in the femoral head (cam type), the acetabulum (pincer type), or both (combined type) cause repetitive impingement during hip movements. This can damage the cartilage and labrum, leading to osteoarthritis.
– Other Secondary Causes: Conditions such as Slipped Capital Femoral Epiphysis, Perthes disease, Inflammatory diseases, and Proximal femoral deficiencies can also lead to early hip osteoarthritis. These conditions affect the normal development or structure of the hip joint, leading to abnormal stress and subsequent degeneration.
Early recognition and treatment of these conditions are crucial to prevent progression.
Myth 5: Hip Joint Pathology Always Requires Total Hip Replacement Surgery, Regardless of Age
Fact: The need for Total Hip Arthroplasty (Hip replacement) depends on several factors, including age, activity level, severity of symptoms, and specific pathology. While severe cartilage loss and “bone-on-bone” arthritis—which have not many choices for long-term cure—may necessitate hip replacement with prosthesis, especially given advancements in surgical techniques and prosthesis longevity, other options are available for less severe cases. If the cartilage is still relatively intact and imaging does not show catastrophic damage, and if patients fail medication or physical therapy, other conservative hip surgical options can be considered:
- Hip Arthroscopy: A minimally invasive procedure to address labral tears, remove bone spurs, or correct impingement.
- Osteotomy Procedures: Surgical realignment to improve hip joint biomechanics.
- Release of Tight Structures: Surgical release of tight muscles or tendons contributing to hip pain.
Treatment should be individualized based on the specific condition and patient needs.

Understanding the facts about hip pain can lead to better management and outcomes. If you experience mechanical repetitive pain, night pain, limited motion at the joint, or signs of inflammation such as redness, swelling, fever, or progressive referred pain to other areas, it’s important to consult a specialist promptly. Early diagnosis and proper management can prevent further complications and improve outcomes.
At Bangkok International Hospital, our team of specialists is dedicated to providing personalized care to help you return to your active lifestyle safely and effectively.