Total Knee Replacement Surgery with Walking Ability within 24 hours
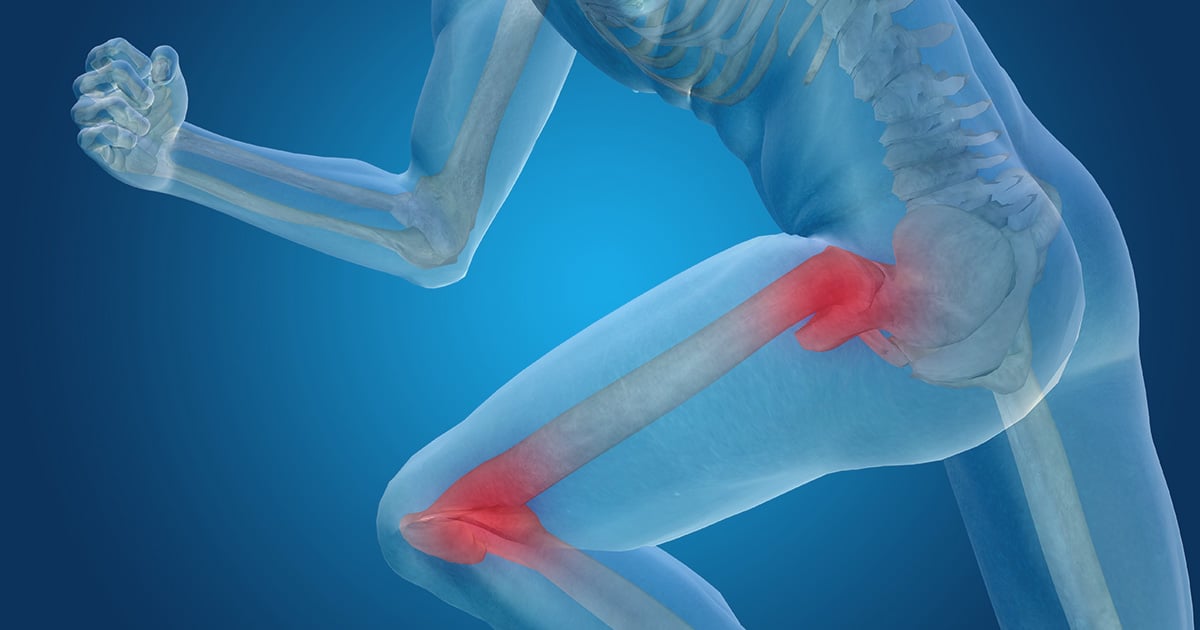
If you have experienced severe pain in your knees while walking, climbing stairs and getting in and out of chairs, knee deformities or chronic knee inflammation that fail to anti-inflammatory medications and injections, these might potentially indicate osteoarthritis of knee. In such a case, you could be a good candidate for total knee replacement surgery.
Besides advancing age, other risk factors for knee osteoarthritis include heredity, gender and history of trauma. Although there is no cure for osteoarthritis of knee, lifestyle changed can slow disease progression. Osteoarthritis of knee can largely impair daily abilities and quality of life. However, a number of people are in fear of having knee operation. Some do not know that total knee replacement surgery is one of the most effective ways to bring back patients to their normal activities in no time.
Total Knee Replacement Surgery
“Total knee replacement surgery seems to be frightening since some patients doubt about curability and inability to walk afterwards. To eliminate this anxiety, Hip and Knee Center at Bangkok International Hospital has come up with a total knee replacement surgery combined with pain intervention technique using radiofrequency abrasion and novel nerve block technique called “adductor canal block” that results in no or less pain, less muscle damages and faster recovery with walking ability within 24 hours after surgery.”
To eliminate suspicion of incurability, a Digital Template Computer Program is used for surgical planning. The program allows the surgeons to customize the size and determine the position of the prosthesis for each individual patient. This, in turn, reduces the possibility of traumatic damage to surrounding areas and prolongs the lifespan of the implants.
Patient’s concern of inability to walk after surgery is dispelled by the fast rehabilitation and recovery program. Patients can usually start walking and restoring full muscle function within 24 hours of surgery. Nearly 100% of patients who receive total knee replacement surgery experience minimal pain and they are able to return to their daily activities within 1.5-3 months.
Key Benefits of Total Knee Replacement Surgery
- Quality Prosthesis
- Minimal pain
- Worry-free with less complications
- Faster Recovery – Walking in 24 hours after surgery*
*Result may vary among individuals
Total Hip Replacement with Advanced Technique – Direct Anterior Approach (DAA)
Hip osteoarthritis often appears in people aged over 40. The genetic abnormality of hip joints, the autoimmune disease of Systemic Lupus Erythematosus (SLE), kidney disease, rheumatoid arthritis or long-term steroid use are major contributing factors. In its late stages, patients often experience chronic hip pain that might radiate to the legs and pain killer drugs might not work anymore. Hip pain usually aggravates when the patients move or climb the stairs. If pain is intensifying, it can disrupt sleeping at night, resulting in limited mobility and poor quality of life.
In the past, patients often avoided traditional hip replacement surgery which involves making a large incision (6 -to 8- inch long) on the side of the hip (lateral approach) or the back of the hip (posterior approach). Both techniques require muscle and tendon detachment from the hip in order to replace the damaged joint. Detachment of these muscles can potentially result in increased pain after operation and prolongs the time to get a full recovery by months or even years. Failure of these muscles to heal properly after surgery may increase the risk of hip dislocation which is the leading cause of hip replacement failure. Undesirable postoperative outcome also includes the risk of unequal length in legs, leading to poor posture and other complications. Nowadays, advanced technology in orthopaedic surgery allows less invasive procedure with improved surgical results and patient satisfactions.
Chat with Us
Total Hip Replacement with Direct Anterior Approach (DAA)
The Direct Anterior Approach (DAA) Cosmetic Incision Hip Replacement Surgery has been increasingly gained popularity in the USA, Canada and Europe as well as Thailand. DAA hip replacement surgery is considered a “minimally invasive surgery” that involves smaller incision (3- to 4-inch long) hidden at the groin beneath the bikini line or a groin crease. This small incision on the front of the hip allows the joint to be replaced by moving muscles aside along their natural tissue planes, without detaching any muscles.
This approach significantly results in less pain, quicker recovery and improved function after surgery. Since the muscles and the tendons are not detached from the hip, hip precautions after surgery e.g. ability to sit with leg crossed or sitting on the floor are typically not required, allowing patients to return to their normal daily activities shortly after treatment with a reduced risk of dislocation. Patients usually require only 2-4 days recovering in the hospital before returning home.
Digital template for surgical planning
Prior to the operation, digital template surgical planning is conducted to select a suitable size of artificial joints for each patient. There is a wide range of artificial joints, such as cobalt chromium or ceramic, while a new version of femoral stems is used to solve the issue of replaced joints sinking later after prolonged use. This planning approach provides better accuracy in examining the length of a patient’s legs and location of hip joints. As the patient lies in the supine position, a C-arm fluoroscopy examination enables accuracy in placing the new joints properly and checking both legs to ensure their equal length.
The latest hip prosthesis
As a pioneer of DAA hip replacement in Asia-Pacific region conducting surgeries over 650 cases, highly experienced team of surgeons at Hip and Knee Center, Bangkok International Hospital uses the latest hip prosthesis (Actis® stem) which is specifically designed to provide ease-of- insertion benefit with improved implant stability with a collar which significantly helps patients restoring their mobility more quickly with confidence and increased satisfaction.
Increased precision with the newest non-invasive hip navigation system
In addition, Velys™ has been deployed as the newest non-invasive hip navigation system to provide the surgeons significant data on cup position, leg length and stem position during procedure. It can help reduce leg length discrepancy and complications related to inaccurate cup placement.
Stay confident with BIKINI incision
Since a surgical mark is made beneath the bikini line, thus shorts or swimsuits can be worn confidently. This approach also decreases the chance of scar formation since the incision follows Langer’s line in which collagen fibers of the dermis layer run parallel to muscles, enabling the wound to heal better. During the procedure, the medical team wears specialised surgical suits to prevent any contaminations, resulting in reduced post-operation infection rates.
“Due to the advancements of navigation system, new generation of prosthesis, less invasive surgical technique, the DAA hip replacement surgery leads to smaller incision, less pain without muscle detachment, less blood loss and lowered post-operative complications as well as faster recovery time and improved mobility with reduced chances of hip dislocation. Besides superior cosmetic effects, patients are not instructed to follow hip precautions after surgery. Bring back their daily life and reboot their bounce.
Novel Pain Intervention Techniques
During and after surgery, inadequate postoperative analgesia can impair rehabilitation, prolong hospitalization and increase the risk of complications, such as myocardial ischemia, myocardial infarction, pulmonary dysfunction, paralytic ileus, urinary retention and thromboembolism. Therefore, acute pain management strategy is crucial. Previous options for postoperative pain control included narcotics, epidural anesthesia and spinal anesthesia.
However, despite the effectiveness of opioids, they also produced undesirable side effects, such as vomiting, constipation, confusion and respiratory depression. This has led to a shift in current pain management regimens. Multimodal analgesic regimen is a regimen where multiple drugs, which act at multiple pain receptors, are used in a lower dosage to reduce opioid side effects. As for knee surgery, an adductor canal block, which is conducted at the end of surgery by a well-trained anesthesiologist is a current gold standard for its pain control. During the procedure, a catheter is inserted into the mid-thigh with the assistance of ultrasound guidance technology, aiming for the saphenous nerve in the knee to be anesthetized.
The adductor canal block in combination with multimodal pain protocols, such as anti-inflammatory agents and nonnarcotic medications can limit the use of narcotics, hence reducing its undesirable side effects. With this intervention technique we can ensure that patients do not endure severe pain and are able to walk within 2 to 3 hours after the operation. The main advantage of this technique is preserving muscle strength in order to facilitate rehabilitation and exercise programs after knee surgery, leading to a quick return to normalcy. Another pain intervention technique is radiofrequency nerve ablation. This minimally-invasive procedure uses conventional or cooled radiofrequency technology to reduce or eliminate chronic pain conditions. This method is often considered an effective option for patients with significant arthritis who are illegible for joint replacement surgery, those who prefer to delay their surgery and patients who are not fit for a major surgery.
During the procedure, with guidance from x-rays and ultrasounds, special radiofrequency needles are placed on nerves that are responsible for pain in the knee or hip. With needle tip placed on the specific area, radiofrequency is started and heats the nerve up to a certain degree. Ablated nerves will stop functioning for a duration of 4 to 6 months up to 2 years, thus pain will be improved. Side effects of this technique are considerably rare due to a precise needle placement technology.
In comparison to other techniques, cooled radiofrequency uses water-cooled technology to safely ablate the nerves that transmit pain signals with lower temperatures (45-60°C). This results in less damage to surrounding tissue and encourages faster recovery, so patients can return to their lives worry free.
Chat with Us