|
Artificial Knee Replacement Surgery Bangkok International Hospital Less pain, fast recovery, able to walk within 24 hours* Call for consultation 1719 or inquire through FB@Bangkokhospital *Results may vary for each individual |
When the knee joint surface is severely damaged due to knee arthritis or accidents, the patient will feel pain when walking or climbing stairs. If the damage is more severe, pain may also be felt while sitting or lying down. Treatment may start from changing knee usage habits, anti-inflammatory medication, or using a walking cane. If these treatments are ineffective, knee replacement surgery (Total Knee Replacement) may be necessary, which involves replacing the damaged surface with a smooth, metal, and plastic one. This allows the knee to function again as normal. Knee replacement surgery is highly successful, with the first surgery conducted in 1968. Since then, the surgery has continually improved in terms of materials used and surgical techniques, resulting in better outcomes.
Anatomy of the Knee
The knee is the largest joint in the body, consisting of three bones:
- The end of the thigh bone (Femur)
- The top of the shin bone (Tibia)
- The kneecap (Patella)
These bones are held firmly together by ligaments, with muscles for movement. The surface of these bones are covered with articular cartilage, which is white, smooth, and acts as a cushion to absorb shocks and smoothens joint movement. Areas not covered by articular cartilage are covered by the synovial membrane, which secretes fluid to lubricate the joint.
Why Does the Knee Pain and Lose Function?
The most common cause is arthritis, which can be due to wear and tear, chronic inflammatory diseases such as Rheumatoid arthritis, and injuries.
- Osteoarthritis
Occurs in patients over the age of 50. It arises from the degeneration of cartilage and the cushioning bone pads, causing the bones to rub against each other. This can cause noise during knee movement, pain, and stiffness when bending the knee.
- Chronic Inflammatory Arthritis
Commonly, rheumatoid arthritis, where the joint’s synovial membrane inflames and thickens, producing more lubricating fluid, resulting in swollen and red knees. Chronic inflammation can lead to bone damage.
- Post-Traumatic Arthritis
Cartilage damage due to accidents, from severe impacts or fractures, which results in uneven joint surface.
Artificial Knee Replacement
Treatment for knee arthritis starts with changing usage habits, reducing activities that cause pressure and shocks like squatting, kneeling, stairs, running, or lifting heavy objects. Taking medication to reduce inflammation in the knee, exercising the muscles for stable movement. If these treatments do not work, considering knee injections to reduce inflammation and lubrication, like steroids or synthetic lubricants. If still ineffective, knee replacement surgery may help reduce pain and enable the patient to resume daily activities.
Knee Examination
Things to examine before knee treatment include:
- Complete health history, symptoms, characteristics of knee pain, and knee function.
- Physical examination, knee function examination, muscle strength around the knee and ligament strength.
- X-Ray to see pathology, knee damage.
- Sometimes special blood tests, X-Rays, or MRI may be required to see the condition of muscles and tissues around the bones.
More than 90% of patients who undergo knee replacement surgery experience reduced pain and can return to normal daily activities. Activities to avoid after knee replacement include high-impact sports that put a strong force on the knee, like running or jumping, which accelerates plastic wear. Avoid squatting, sitting cross-legged, especially using squat toilets should be strictly avoided.

Preparation before Surgery
- General physical examination by an internal medicine doctor to assess readiness before surgery, and may have to be re-examined by a specialist, such as a cardiologist.
- Laboratory tests, blood tests, urine tests, and X-Rays.
- Preparation of the surgery area, check skin condition on the knees and legs. If there are any abnormalities related to inflammation or swelling, report to the doctor before surgery.
- Blood preparation, as knee replacement is major surgery involving significant blood loss, may require blood transfusion during or after surgery. It’s recommended to donate the patient’s own blood for use in the surgery, donating 3 – 4 weeks before surgery, with the final donation no less than 2 weeks before surgery.
- Preparation regarding the patient’s regular medication. The patient must inform the doctor about all medications being taken, as some drugs, like those affecting blood clotting, aspirin, some anti-inflammatory drugs, need to be stopped before surgery.
- Dental examination, significant dental work like root canal treatment, tooth or gum infection could lead to infection in the artificial joint. Therefore, it’s advisable to complete all major dental treatments before surgery.
- Preparing about the urinary system. It’s important to address chronic urinary infections, like from an enlarged prostate, as urinary system infections could lead to infection in the artificial joint.
- Preparing the home environment and help for the post-surgery period. The patient will be able to move with support devices but initially will need assistance for certain activities like bathing, cooking, shopping, or laundry. Home and environmental modifications are recommended for post-surgery:
- Installing bars along the bathroom to aid in walking.
- Ensuring stair railings are sturdy.
- Having rails around the toilet area to assist in getting up.
- Using a plastic chair during showering.
- All rooms should be on the same level to avoid using stairs.
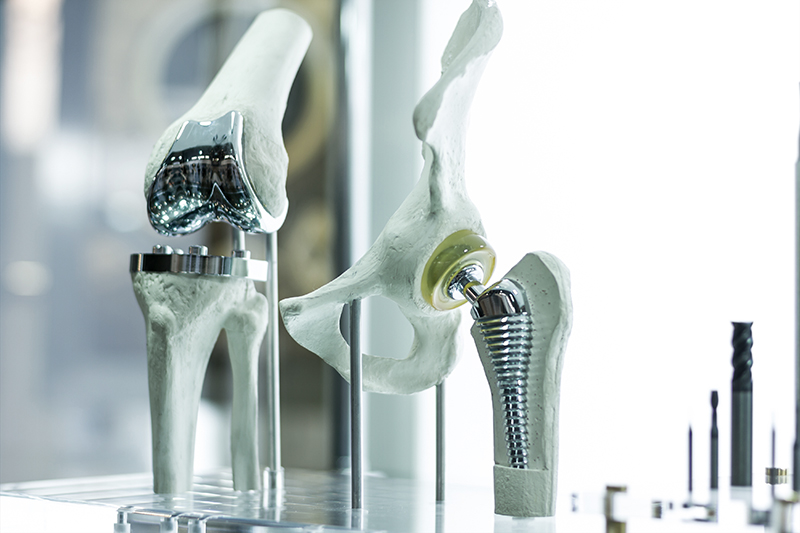
Types of Knee Prostheses
- Total Knee Replacement Replacing the entire knee surface, both the end of the thigh bone (Femur) and the top of the shin bone (Tibia), with metal surfaces separated by plastic padding.
- Unicompartmental Knee Replacement Replacing just one side of the knee surface specifically where the deterioration occurs. The advantage is smaller incisions, less bone and tissue cutting, resulting in less pain and quicker muscle recovery. However, it’s only suitable for knees with limited damage on one side.
Artificial Knee Replacement Surgery
Patients usually arrive at the hospital in the morning of the surgery day. Afterwards, the anesthetist will visit the patient to explain anesthesia options, which are general anesthesia and spinal injection, the choice of which depends on the anesthetist’s discretion.
The surgery takes about 3 hours, where the damaged joint surface is replaced with artificial surfaces made of metal, with plastic padding in between to absorb shock and reduce friction between the surfaces. After the surgery, the patient stays in the recovery room for 1 – 2 hours. Once awake from anesthesia, they are moved to their room. Typically, patients stay in the hospital for 5 – 7 days post-surgery, during which they may have:
- A urinary catheter to manage bodily fluids accurately.
- An IV for blood, saline, and antibiotics administration shortly after surgery. Patients may feel nauseous and disoriented, so saline is administered until they can eat properly on their own.
- Antibiotics are normally given 1/2 – 1 hour before surgery and continued for 1 – 2 days post-surgery.
- Due to significant blood and muscle loss during surgery, blood transfusions may be necessary.
- A tube to drain blood from the surgical area is inserted, usually for 2 – 3 days until post-operative bleeding stops.
- After surgery, patients are encouraged to breathe deeply and cough frequently to help expand the lungs, preventing pneumonia, and may use a machine that helps move the knee (Continuous Passive Motion – CCPM) to aid in knee movement. On the 2nd – 3rd day, patients begin knee exercises and start to sit-up, stand, and walk with the help of a physical therapist. Once able to move independently, with no infection at the surgical wound, patients can go home, usually within 5 – 7 days.
Complications After Knee Replacement Surgery
- The most important complication is infection, which is quite low, about less than 2%.
- Cardiac complications due to significant blood loss and transfusion may lead to heart failure.
- Deep vein thrombosis (DVT) where a clot could travel to heart muscle or lungs causing circulatory failure. It’s more common in Caucasians but can also occur in Asians and Thais. Prevention includes moving both legs as soon as possible, which improves blood flow and reduces clotting. Medication to prevent clotting is usually started on the 1st or 2nd day after surgery and continued for about 10 – 14 days post-surgery.
Signs of Deep Vein Thrombosis
- Pain in the calf
- Pain, swelling, redness above or below the knee
- Increased swelling in the calf, ankle, and foot
Patients Suitable for Knee Replacement Surgery
- Severe knee pain that interferes with daily activities, like severe pain while walking, climbing stairs, standing, or sitting.
- Pain in the knee while resting, such as pain while sleeping.
- Inflamed, red knee with frequent and chronic symptoms.
- Knee deformity, e.g., bow-legged or knock-kneed, etc.
- Difficulty in moving the knee, trouble bending or straightening.
- Other treatment methods, such as changing usage habits, medications, or knee injections, have failed.
Knee replacement surgery is usually performed on patients aged 60 – 80 years. Each case is considered individually depending on the symptoms and the severity of the disease.